Histamine Intolerance: What It Is & How to Combat It
More is not always better. Too much of something good for you can be detrimental to your health and wellness.
This happens to be true for histamine, the culprit of a lesser-known condition afflicting a growing number of Americans: histamine intolerance.
What is histamine?
To understand histamine intolerance, first we must understand the chemical responsible for this condition. Most of us are familiar with antihistamines (perhaps a little too familiar during allergy season!), but what is histamine itself?
Histamine is an organic compound involved in several essential bodily functions:
neurotransmission: it carries messages between nerve cells
digestion: it triggers the release of stomach acid to help break down food
immune response: releases an inflammatory response following injury or allergic reaction
sleep: it circulates throughout body to regulate our sleep/wake cycle
Normal levels of histamine are vital to human life.
But when this chemical builds up in our body or we are unable to properly break it down, histamine becomes problematic.
What is histamine intolerance?
Don’t be fooled by the name—histamine intolerance is not a sensitivity or allergy to histamine, but rather the accumulation of too much histamine (more than our bodies can handle). Because histamine receptors are found throughout the body, it’s no surprise that this medical condition produces a whole gamut of symptoms.
What are the symptoms of histamine intolerance?
The symptoms of histamine intolerance vary, depending on the level of histamine built up in the body. Often, these symptoms mimic those of an allergic reaction. Symptoms of histamine intolerance may include (but are not limited to):
Gastrointestinal
diarrhea
irritable bowel syndrome (IBS)
indigestion, stomach cramps or pain
gas or bloating
heartburn
nausea and/or vomiting
Neurological
chronic headache
mood swings
brain fog
unexplained anxiety
Cardiovascular
irregular or increased heart rate
low blood pressure
Skin
rashes, hives, itching
eczema
flushing (specifically in the head and chest region)
Ear, nose & throat
sneezing
itching
congestion or sinus issues
swelling or inflammation
Other
dizziness
fatigue
shortness of breath
sleep problems
menstrual pain
Due to the wide range of possible symptoms, histamine intolerance can often be difficult to diagnose. Understanding the cause of histamine intolerance is fundamental to recognizing and properly treating this condition.
What causes histamine intolerance?
So what leads to the build up of histamine in the bloodstream?
Nearly all foods and drinks contain histamine. These dietary sources are usually broken down and rapidly detoxified by the enzymes diamine oxidase (DAO) and histamine n-methyltransferase (HNMT). A combination of genetic, gastrointestinal and environmental factors may decrease the effectiveness or abundance of these enzymes, or increase the amount of histamine released in the body.
Factors that contribute to the interference of DAO and HNMT enzymes include:
genetic predisposition
chronic stress
intestinal conditions or injuries, such as small bowel intestinal overgrowth (SIBO), leaky gut or gastrointestinal bleeding
prescription and over-the-counter drugs, such as commonly used anti-inflammatories (NSAIDs)
alcohol
histamine-rich diet
vitamin deficiencies
allergies
When the body is unable to break down ingested histamine, the chemical leaks through the intestinal wall and builds up in the bloodstream (resulting in a systemic immune response).
How to test for histamine intolerance
The first step to diagnosing histamine intolerance usually involves ruling out other possible medical issues and allergies that may be triggering your symptoms. An elimination diet may be recommended to check for food allergies and intolerances. If a histamine intolerance is suspected, consider keeping a food diary to identify symptoms corresponding to dietary changes.
Additionally, the following tests may be ordered by a physician:
blood test to check for low DAO (diamine oxidase) levels
blood test to check for serum tryptase levels to rule out a mast cell disorder (mast cells are responsible for releasing histamine)
skin-prick test for histamine intolerance (not widely used due to lack of reliability)
A reduction in dietary histamine intake (resulting in improved symptoms) is often the gold standard for both diagnosis and treatment.
How to treat histamine intolerance
Treating histamine intolerance involves avoiding triggers and rebuilding healthy gut flora. Because almost all foods and beverages contain histamine, focusing on diet is key.
How to combat histamine intolerance with diet
First, what not to eat: Avoid foods and beverages that are a) histamine-rich, b) trigger the release of histamine in the body or c) inhibit production or effectiveness of DAO or HNMT enzymatic activity.
Avoid high-histamine foods
Many foods and beverages naturally contain high levels of histamine (some due to aging, curing, and fermentation processes):
alcohol, kombucha and other fermented beverages
red wine vinegar
canned, pickled and fermented foods or dairy products such as kimchi, sauerkraut and yogurt/kefir
aged cheeses
smoked meats such as sausage, bacon and salamis
canned and smoked fish
dried fruits
most citrus fruits, pineapple, bananas, strawberries and cherries
spinach, eggplant, mushrooms, tomatoes and avocados
legumes (such as lentils, beans and chickpeas)
peanuts
chocolate and cocoa
green tea
chili powder, cinnamon and cloves
Histamine levels also increase in food over time. Consume fresh foods quickly and freeze leftovers to minimize this risk.
Avoid histamine-releasing foods
Some foods (regardless of their respective histamine levels) work to release histamine in the body:
alcohol
shellfish
most citrus fruits, pineapple, bananas, strawberries and papaya
tomatoes and avocados
beans
nuts
chocolate and cocoa
Avoid DAO/HNMT inhibitor foods
Other foods and beverages specifically interfere with the DAO and HNMT activity:
alcohol
green, black, and mate tea
energy drinks
dairy products such as some yogurts and raw egg whites
As you may have noticed, many foods and beverages are cross referenced in the above not-so-histamine-friendly lists (a double or even triple whammy!). Start by limiting these triggers if excluding them altogether proves a challenge.
So, you’re probably wondering: what can I eat? If you suspect a histamine intolerance, try a diet focused on fresh meats, vegetables, fruits and whole grains.
Focus on low-histamine foods
fresh meats and fish
cooked eggs, butter, cream cheese
most cooking oils, such as coconut and olive oil
apple cider vinegar
most organic vegetables and fruits, excluding those listed above
gluten-free whole grains such as brown rice, quinoa and oats
dairy substitute beverages, such as coconut and rice milk
most herbal teas, excluding those listed above
Not sure where to start? Here are some of our favorite histamine-friendly recipes:
Histamine-friendly Nomato Sauce
// Histamine Friendly Kitchen
Low-histamine Sweet Potato Soup
// Lectin Free Mama
Overnight Oats
// Simply Connie
How to combat histamine intolerance with supplements
While a low-histamine diet is nutrient-rich, you may also want to consider incorporating some vitamins and minerals into your restricted diet. The following work together to help support enzymatic activity, lower histamine levels and reduce inflammatory response:
vitamin B-1, B-6, and B-12
vitamin C
magnesium
manganese
calcium
copper
zinc
folic acid
Other beneficial supplements include DAO enzymes (found at your local health foods store), natural antihistamines (e.g. stinging nettle, bromelain, butterbur, and quercetin) and probiotics (more about our favorite probiotics here—just remember to limit those ferments in your low-histamine diet!). Avoid medications associated with histamine intolerance (such as over-the-counter anti-inflammatories) and opt instead for natural remedies like ginger and turmeric.
With the appropriate dietary changes and nutritional support, histamine intolerance can be properly managed within weeks to months.
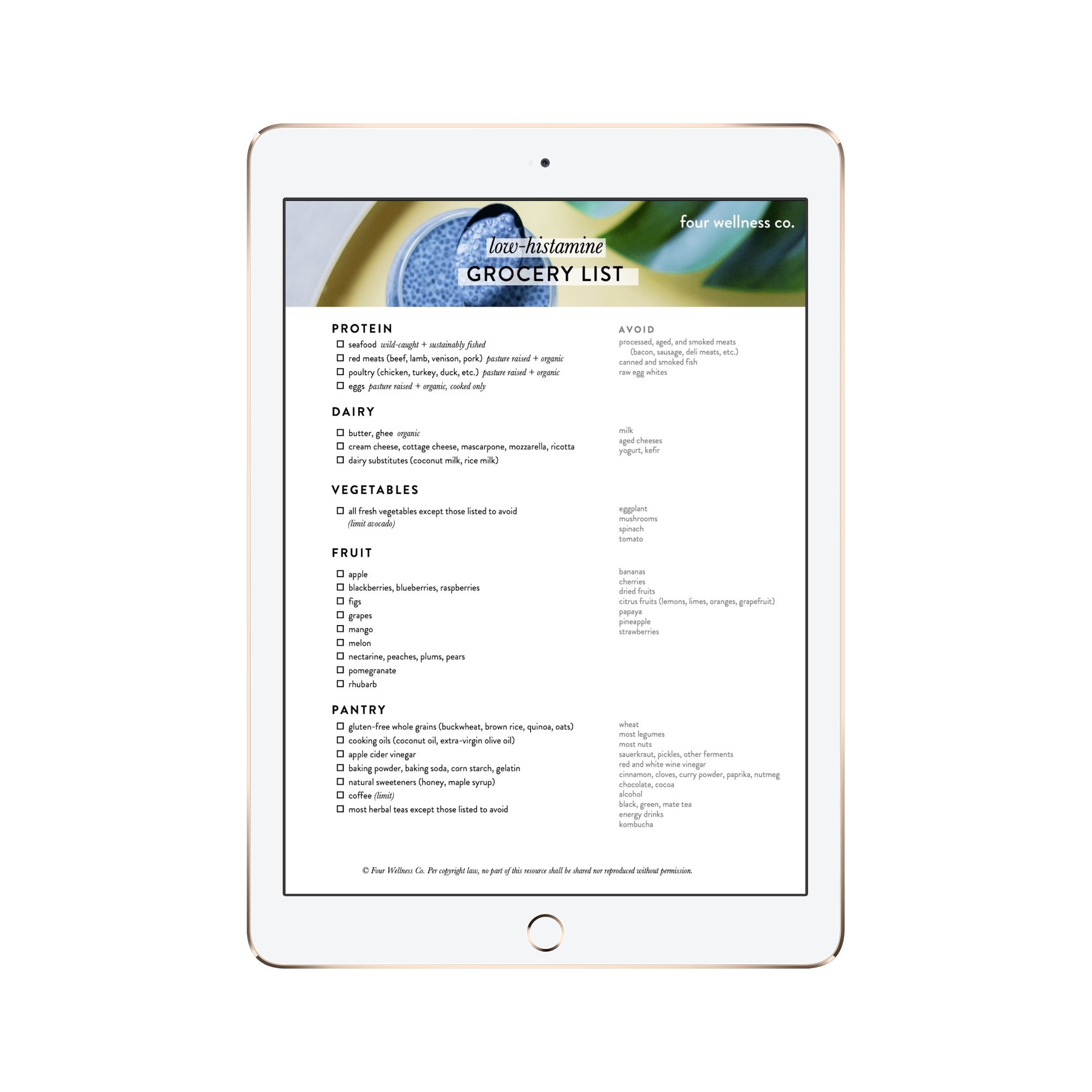
Low-histamine Grocery List
Grab our printable checklist of what to purchase (and what to avoid!) while grocery shopping for a low-histamine diet.
It’s part of our Wellness Library of healthy living guides + resources:
FOUR WELLNESS TIP
Combat histamine intolerance with a diet of fresh, low-histamine whole foods.